24/05/2021
Samhita Ghanathay
- This is an online E log book to discuss our patient's de-identified health data shared after taking her/his guardian's signed informed consent.
- Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
- This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
50-Years Old Female With Fever, Cough and Shortness Of Breath
I've been given this case to solve, in an attempt to understand the topic of "patient clinical data analysis" to develope my competency in reading and comprehending clinical data - including history, clinical findings, investigations - and come up with diagnosis and treatment plan.
Following is a brief about the case,
(History as per date of admission).
CHIEF COMPLAINTS:
A 50 year old female patient came to the General Medicine OPD on 13/05/2021 with chief complaints of :
- Fever since 2 days
- Cough since 2 days
- Difficulty in breathing since 2 days
HISTORY OF PRESENT ILLNESS:
The patient was apparently asymptomatic 2 days ago, when he developed
- Fever, which was insidious in onset, gradual in progression and not associated with chills and rigor.
- Cough with expectoration
- Dyspnoea, of grade 2.
There were no aggravating or relieving factors.
There were no associated features.
No history of vomitings, chest pain, palpitation, sweating, loose stools.
HISTORY OF PAST ILLNESS:
- Known case of Hypertension since 2 years - on regular medication
- No history of Diabetes, Asthama, Epilepsy, Tuberculosis.
- No history similar complaints in the past.
- No history of any previous surgeries.
PERSONAL HISTORY:
- Diet - Mixed
- Appetite - Reduced
- Bowel and Bladder - Regular
- Sleep - Normal
- No known allergies
- No addictions
FAMILY HISTORY:
No history of similar complaints in the family.
GENERAL EXAMINATION:
The patient is conscious,coherent and cooperative; well oriented to time,place and person.
He is sitting comfortably on the bed.
He is moderately build and well nourished.
- Pallor-absent
- Icterus-absent
- Clubbing-absent
- Cyanosis-absent
- Lymphadenopathy-absent
- Edema - absent
Vitals:
- Temperature - 99* F
- Pulse rate - 102/ minute
- Respiratory rate - 40/minute
- Blood pressure (left arm) - 120/70 mm of Hg
- SpO2 (At room air) - 80%
- GRBS - high
SYSTEMIC EXAMINATION:
CVS: S1 and S2 heard. No addded thrills or murmurs heard
RESPIRATORY SYSTEM:
Normal vesicular breath sounds heard.
Dyspnoea of grade 3 developed.
ABDOMEN:
Soft and non-tender.
no organomegaly seen
CNS:
Conscious and coherent.
Normal sensory and motor responses.
INVESTIGATIONS:
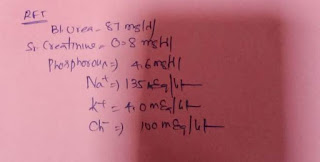
Investigations ordered: CBP, CRP, ESR, Xray, ECG, D-dimer, Serum LDH, Serum Ferratin, LFT, RFT, FBS, PLBS.
Reports available have been presented below:
- ECG:
PROVISIONAL DIAGNOSIS:
Severe pneumonia secondary to COVID-19 infection with Diabetes Ketoacidosis.
TREATMENT:
- O2 inhalation to maintain SpO2 >90%
- Tab.Clexam- 40mg
- Inj.Dexamethasone - 6mg/IV/OD
- Tab.MVT - PO/OD
- Inj.Pantop - 40mg/IV/OD
- Nebulication with Duolin, Budecot, Mucomist - 8th hourly
- Tab.Limcee PO/OD
- Tab.Augmentin - 625mg
Despite above measures, with severe pneumonia secondary to Covid-19 and uncontrolled blood sugar levels, the patient's O2 dropped to 30% at 15L oxygen. BP and PR were not measurable. She was intubated and CRP was initaited at 11AM.
The patient could not be revived and was declared dead at 11:46 AM on 15/05/2021.
Immediate cause of death: Type 2 respiratory failure
Antecedent cause of death : Severe Covid-19 pneumonia with uncontrolled blood sugars.
RELATED QUESTIONS:
- What is the possible cause of sudden increase in blood suger levels, considering she was not a known case of Diabetes?
NOTES:
- Patient came to the hospital on 3rd day of symptoms and was admitted on the same day.
- Duration of Hospital stay: 3 days
- Reason for discharge: Death of patient
- Severity of disease : Severe.
I would like to thank Dr.Rakesh Biswas sir for providing me with this oppurtunity to learn better and Dr.Saicharan sir for guiding me during the case.



Comments
Post a Comment