15/07/2023
Samhita Ghanathay
- This is an online E log book to discuss our patient's de-identified health data shared after taking her/his guardian's signed informed consent.
- Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
- This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
55 year old male with complaints of shortness of breath and pedal oedema.
I've been given this case to solve, in an attempt to understand the topic of "patient clinical data analysis" to develope my competency in reading and comprehending clinical data - including history, clinical findings, investigations - and come up with diagnosis and treatment plan.
Following is a brief about the case,
(History as per date of admission).
CHEIF COMPLAINTS:
A 55year old male male, resident of Suryapeta, who stays at home for past 10 years, was brought to the casualty with chief complaints of:
* Shortness of breath since 15 days
* B/L pedal oedema since 7 days
* Reduced urine output since 7 days
HISTORY OF PRESENT ILLNESS:
The patient was apparently asymptomatic 15 days back, then he developed SOB(grade I-II), that was insidious in onset, gradually progressing, no aggravating or relieving factors present.
He C/O B/L pedal oedema since 5 years, aggravated since last 7 days, pitting type, extending upto the knee. Not relieving on medication.
C/O reduced urine output since 7 days.
No C/O chest pain, palpitations, orthopnea, PND.
No H/O fever, burning micturition, loose stools, vomiting.
No C/O pain abdomen.
PAST HISTORY:
Daily routine:
10 years ago, he used work as as a farmer.
Woke up at 5am, had breakfast around 7am and left for work by 8am. He packed his lunch which he ate at his workplace around 1pm, and came home by 7pm.
He ate at 8pm and slept at 10pm.
10 years back, he met with an accident while attending a funeral and had a fractured left femur that was conservatively treated. So he took a break from work.
A few months later, he slipped and fell at his house and had a similar fracture in the right hip joint that was also treated conservatively.
After this, he stopped working as he needs support of sticks to walk around.
Now his routine has changed as follows :
Wakes up at 6am, has breakfast at 7am and sits in the veranda for a while.
Then goes inside his house, eats at 1pm, sits with wife/sone neighbour for the afternoon,has dinner at 8pm and sleeps at 10pm.
* There is no history of similar complaints in the past.
* he was diagnosed with CKD 1 month ago, is on irregular medication
* he is not a known case of Diabetes, Hypertension, Asthama, Epilepsy, Tuberculosis.
* No history of any previous surgeries.
PERSONAL HISTORY:
* Diet - Mixed
* Appatite - Normal
* Sleep - Reduced
* Bowel and Bladder - Reduced urination, normal bowel.
* Allergy - None
* Addictions
- Alcohol - about 90ml per day since his teenage.
- Bedi - 1 packet per day since his teenage.
FAMILY HISTORY:
No history of similar complaints in the family.
GENERAL EXAMINATION:
The patient is conscious,coherent and cooperative; well oriented to time,place and person.
He is sleeping comfortably on the bed.
He is moderately build and well nourished.
* Pallor - present
*Icterus- present
*Clubbing-absent
*Cyanosis-absent
*Lymphadenopathy-absent
*Edema - B/L pitting type present, extending upto the knee.
Vitals:
- Temperature -afebrile.
- Pulse rate - 94/ minute
- Respiratory rate - 20/minute
- Blood pressure (left arm) - 100/60 mm of Hg
- GRBS - 105 mg/dl
SYSTEMIC EXAMINATION:
CVS: S1 and S2 heard. No addded thrills or murmurs heard
RESPIRATORY SYSTEM:
Normal vesicular breath sounds heard.
ABDOMEN:
*non tender
*soft
CNS:
Conscious and coherent.
Normal sensory and motor responses.
INVESTIGATIONS :
ECG at 2am
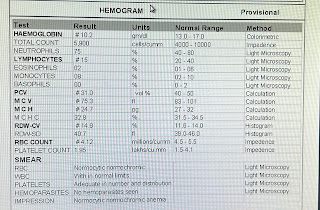
Hemogram - increased lymphocytes
CUE - normal
LFT -
DB - increased
Alk Phos- increased
TP - increased
RFT-
Urea - increased
Creatinine - increased
Uric acid - low
S.Creat - increased
B.urea - increased
Chest x-ray


















Comments
Post a Comment