28/07/2023
Samhita Ghanathay
- This is an online E log book to discuss our patient's de-identified health data shared after taking her/his guardian's signed informed consent.
- Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
- This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
40 year old male with complaints of pain abdomen.
I've been given this case to solve, in an attempt to understand the topic of "patient clinical data analysis" to develope my competency in reading and comprehending clinical data - including history, clinical findings, investigations - and come up with diagnosis and treatment plan.
Following is a brief about the case,
(History as per date of admission).
CHEIF COMPLAINTS:
A 40 year old male resident of Suryapet, farmer by occupation, came to OPD with complaints of pain abdomen since 2 days.
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 2 days back then developed pain over the left hypochondriac region, that was insidious in onset and gradually progressive, radiating to the right hypochondriac region.
C/o vomiting since yesterday, 3 episodes, watery in consistency, non-blood stained, non-foul smelling.
H/o Burning micturition since 2 days.
C/o SOB , palpitations, orthopnea, PND.
No H/o fever, cold, cough.
No H/O decreased urine output ,loose stools
PAST HISTORY:
Not a known case of HTN,DM,Asthma,Epilepsy.
PERSONAL HISTORY:
* Diet - Mixed
* Appatite - Normal
* Sleep - Normal
* Bowel and Bladder -Regular.
* Allergy - None
* Addictions -Alcohol addiction since 10 years last consumption was 2 days back.
FAMILY HISTORY:
No history of similar complaints in the family.
GENERAL EXAMINATION:
The patient is conscious,coherent and cooperative; well oriented to time,place and person.
* Pallor - absent
* Icterus- absent
* Clubbing-absent
* Cyanosis-absent
* Lymphadenopathy-absent
* Edema - absent
VITALS:
* Temperature - 98.6 F.
* Blood pressure - 140/90 mmHg
* Pulse rate - 85/ minute
* Respiratory rate - 18/minute
SYSTEMIC EXAMINATION:
CVS:
S1 and S2 heard.
No addded thrills or murmurs heard
RESPIRATORY SYSTEM:
Normal vesicular breath sounds heard.
Bilateral air entry present.
ABDOMEN:
INSPECTION:
shape of abdomen - distended
umbilicus -central
no sinuses
No scars
PALPATION:
Tenderness+ over hypochondriac region
Fluid thrill +
Puddle sign +
PERCUSSION:
No shifting dullness
AUSCULTATION:
Bowel sounds +
CNS:
Conscious and coherent.
Normal sensory and motor responses.
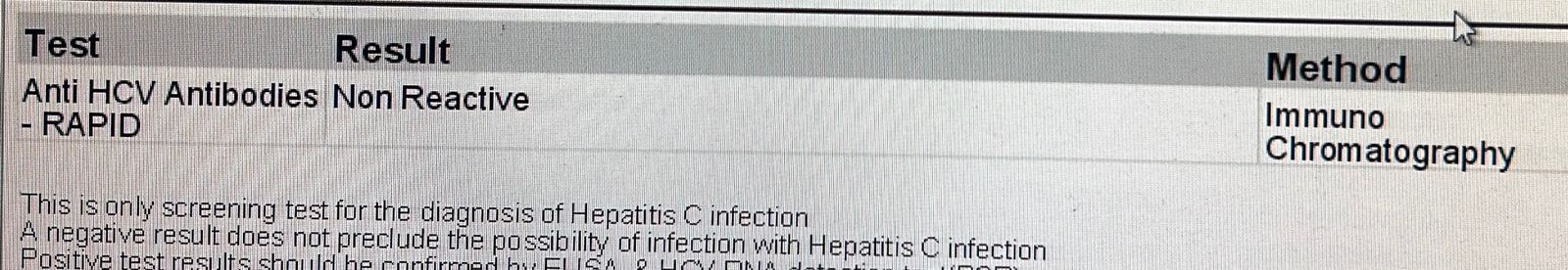
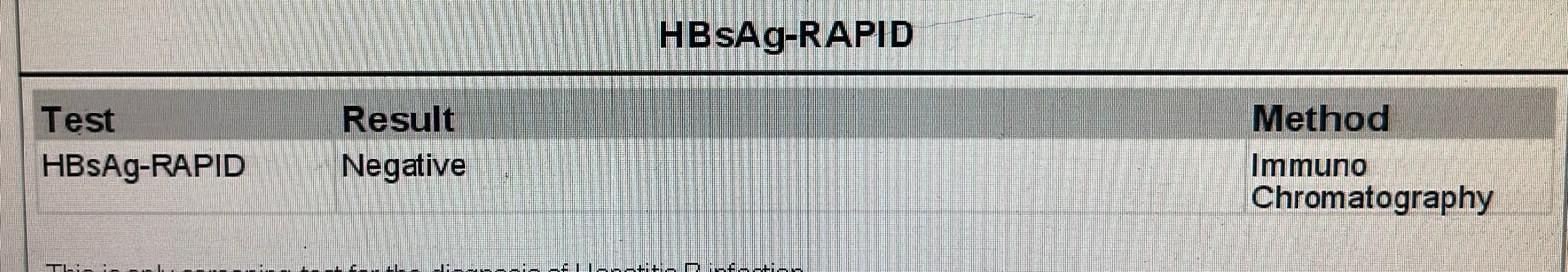
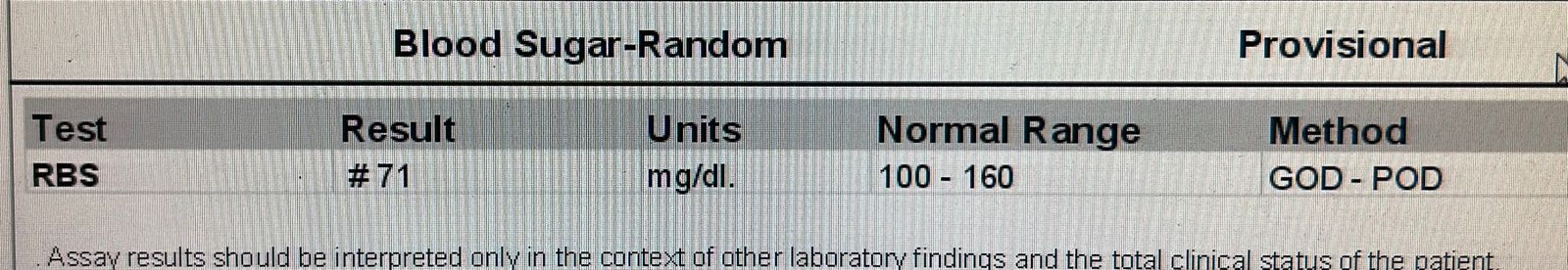
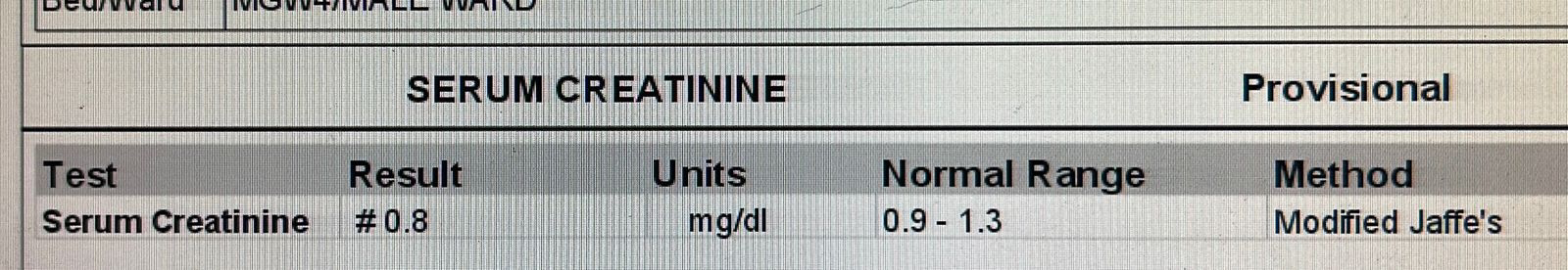
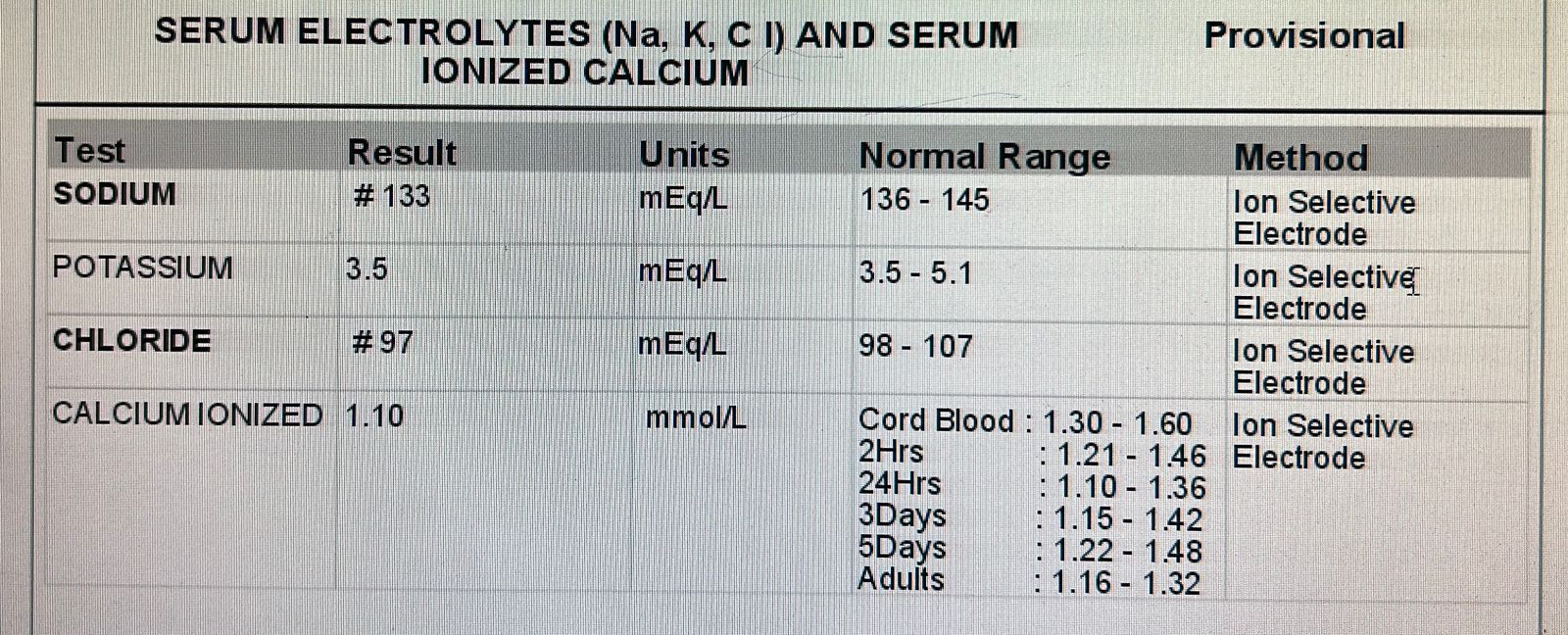
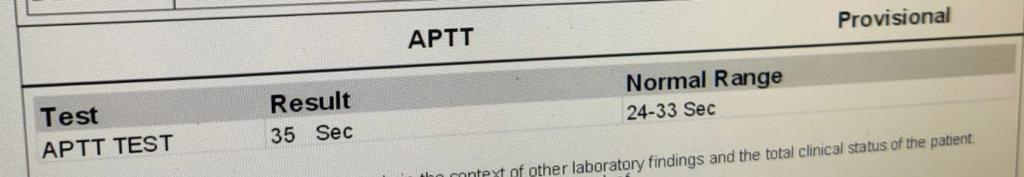
INVESTIGATIONS:











Comments
Post a Comment